WHAT IS GENE THERAPY?

Contributing Author: Norman Rogers, Former Business Development Lead at AGT ™
Gene therapy is a tool to modify the composition and expression of human DNA. Our DNA is the software that codes for every mechanism in the human body. Many diseases are caused by a single error in this code. Until recently, there was no way to directly correct DNA so diseases had to be treated after the harmful effect had begun.
As an example, Phenylketurnuria (PKU) is a disease wherein the PAH gene (phenylalanine hydroxylase) is less effective than standard. PAH processes an essential building block the human body requires to build proteins. Without a working copy of this gene, PKU could be treated in several ways. The enzyme might be replaced by frequently injecting the patient with a purified PAH enzyme. Alternatively, a molecule that assists in the enzymatic process could be used to drive the reaction. Or, a patient could manage a very meticulous diet for life avoiding the molecule that builds up in the body. These treatments serve to treat the problem rather than solve it and are not complete solutions for the patient.
Gene therapy, however, has the potential to replace the broken enzyme in the correct tissue, without a need for a lifelong regiment of diet and drugs. In this case, the difference between small-molecule treatment and gene therapy is analogous to the difference between pouring brake fluid into a car with a leak for years and replacing the leaking line. One solution is temporary and an accident waiting to happen. The other solves the problem at the cause.
DNA-Designed Processes
Viruses attack specific tissues in the body. Some attack nerve cells, others attack immune cells or the liver. That, in general, is bad. Viruses attack a tissue, insert DNA code with instructions to make more virus, and the immune system has to clean up the mess. What if, instead of inserting instructions to replicate themselves, viruses inserted code that improves the body. Scientists now have the ability to modify the instructional package within a virus and deliver only the DNA they design. This ability to deliver custom strings of DNA packaged within a virus is the core of viral vector technology. Scientists are now able to convert viruses into updates for the human software, DNA.
Time, Investment the key to improvement
Today there are still fewer than 10 FDA approved gene therapies (first approval in August 2017). Below are two examples of how gene therapy works, but it is important to realize today’s tools and methods will only improve with time and investment.
Viral vectors are the primary tool for delivering genes to the human body. Adeno-associated virus (AAV) and lentivirus are the most common viral vectors for use in humans. Both are derived from viruses that have been heavily modified to remove any nefarious code. The code that replicates the virus is removed along with potentially deadly signals, which might promote the production of genes within the genome causing harm.
Within these viral vectors, researchers are able to package beneficial genes to be delivered into the cell. These genes could be used to turn off, turn on, or install a new gene. The package viral vectors deliver is custom designed by the developer. Instead of delivering copies of the viral genome, these viral vectors can deliver life-saving changes or updates to one’s software.
AAV Could Correct SMA gene
Recently, the FDA approved a gene therapy for spinal muscular atrophy (SMA). SMA is a deadly disease that robs a child of the ability to roll over or sit up, and eventually the ability to breath. Untreated patients with a SMA 0-1 diagnosis had a life expectancy of fewer than four years. The mutated gene in patients is SMN1, a single gene associated with the survival of motor neurons.
To correct this disorder, biotech companies, in a series of baton passes (RegenexBio to Avexis to Novartis), developed an AAV containing a correct copy of the SMN1 gene and delivered it as an intravenous infusion. The virus itself hones to the brain and spinal cord cells, correcting the defect in motor neurons.

CAR-T Promising
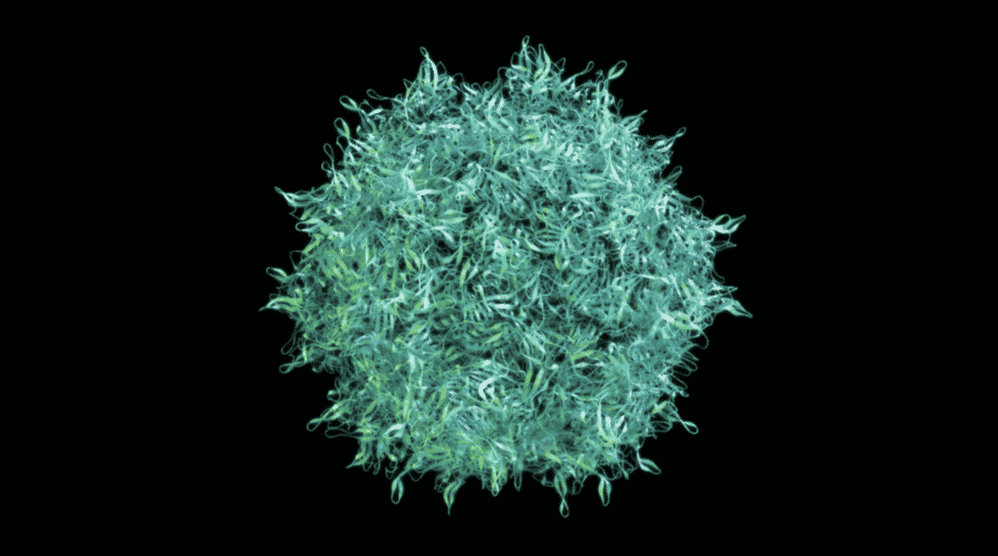
In the past three years, two CAR-T therapies were FDA approved. In these therapies, white blood cells drawn from the patient are genetically modified in a cell processing machine (fancy petri dish) with a lentiviral vector, then re-infused into the body to attack a cancerous target.
Researchers identified that certain cancers express natural receptors on the surface of the cell. These receptors on the surface of cancerous cells make them potential targets for CAR-T. Researchers modify the natural targeting system of immune cells to attack and kill cancers with the receptor targets on their surface. To accomplish this, they use a lentivirus to permanently install code for a cancer-targeting receptor on the surface of immune cells.
With a cancer-targeting receptor added to the surface of the immune cell, these modified immune cells become cancer fighting bots in the body. Because the process for CAR-T is expensive and has long-term side effects today, only formerly incurable forms of cancer are addressable with this technology. Of the two formerly incurable cancers with CAR-T treatments available, ~60-90% patients experience complete remission after a single treatment.
Cost?
The cost of any technology is very high when it first emerges. Currently, there are only a few FDA-approved gene therapies. Below is a list of the costs for the currently approved gene therapies. Although these prices seem astronomical, it is expected the cost will decline as therapies improve and as a market emerges around manufacturing, logistics and reusable components.
- KYMRIAH (tisagenlecleucel)
Novartis Pharmaceuticals Corporation $475,000 - LUXTURNA
Roche, Inc. $850,000 or $425,000 per eye - YESCARTA (axicabtagene ciloleucel)
Gilead, Incorporated $373,000 - ZOLGENSMA (onasemnogene abeparvovec-xioi)
Novartis, Inc. $2,100,000
And Now for the Upside
One compelling feature of gene therapy, when compared with traditional drug development, is that much of the manufacturing does not require a unique facility. Making a batch of viral vector for SMA one month and viral vector for PKU the next is possible with few changes to the manufacturing facilities.
This allows manufacturers to:
- Scale their ability with multiple customer contracts
- Spread the cost among them
- Cancels a single winners potential to dominate the market based on infrastructure costs.
Dream Big
Today, there are several competing companies that produce GMP viral vector. Demand is much higher than supply, but the entrance of new competitors and scaling of existing manufacturers are rising to meet the demand.
The most convincing argument for scaling this industry is inherent to the technology. Imagine a team of gene therapy developers had been awarded FDA approval for a virus that delivered a corrective gene into the liver. Would they:
- Decorate a dartboard with names of diseases and choose their next target with the throw of a dart?
- Or
- Seek out another disorder in which a gene delivered to the liver might be corrective and reuse everything but the payload they had developed over years and several million dollars?
It takes a few minutes to even unpack how many potential problems and pitfalls are avoided by developing a “drug” when only the genetic payload changes. There will be efficiency causing overlap in:
- Development
- Safety
- Regulation (FDA)
- Manufacturing
- Viral targeting
- Viral expression.
Costs Could Halve
Efficiency in gene and cell therapy development alters the strategic model for pharmaceutical companies. Today the strategy of pharmaceutical companies is to create disease based monopolies and manage their own strategic marketplaces. But the development of gene therapies don’t follow disease threads but rather the capabilities of the technology. In other words, gene therapy will by its nature break up these disease based monopolies by developing where the technology is capable rather than what is strategic to the company. Drug companies will have to find a new way to protect their domain or suffer surprising market upsets.
Gene therapy resembles software development more than traditional drug development. Fortunes will be won and lost, but overtime cost trends will carry inversely to that of technological improvements within the industry. As technology doubles, costs will halve.
A View Down the Road
It is easy to predict the ~7000 monogenic (one gene is broken) diseases will be treated, if not cured, by this new type of medicine. Although most of these diseases are quite rare, when combined they represent one out of 10 people. Improvement in 10% of these patients is a profound outcome, but that is just the beginning! Preventative medicine has weighty impacts when compared to that of reactive medicine. How might we get ahead of disease in the future?
We know that some people are more prone to heart disease than others. Although not traditionally thought of as a genetic disorder, the build-up of cholesterol plaque in the walls of blood vessels might be corrected with a protein that packages fats more efficiently in the liver or administration of a gene to the cellular walls of the blood vessels.
We know some people are not as prone to cancer. Perhaps those subgroups have genes that will aid in a discovery that improves the action or longevity of the subset of the immune system that already naturally manages malignancies in the body (ImmunoTox). Perhaps, instead of chemotherapy, a frozen bank of our young immune cells could be separated, modified, and applied against cancers with a specificity we have yet to dream of…
Anything is Possible!
We are in a transition from analog drugs to digital drugs. What is possible in an environment in which the power of the technology doubles and the cost halves? Anything!