Why Is It So Difficult to Find an HIV Cure?

The silent HIV epidemic has been ongoing for 4 decades.
AIDS-related illnesses have claimed over 32 million lives since the beginning of the HIV epidemic in 1981. The death toll, societal impact, and economic effects of the HIV epidemic have made HIV/AIDS one of the greatest public health threats the world has ever known. Governments, companies and private individuals have collectively spent trillions of dollars on the development of effective treatments and the search for an effective vaccine or a cure. Today, antiretroviral medications (ART) make HIV a manageable condition, but neither a vaccine nor a cure are available. However, the fight for a cure isn’t over, and new biotechnologies may finally provide a definitive remedy for people living with HIV.
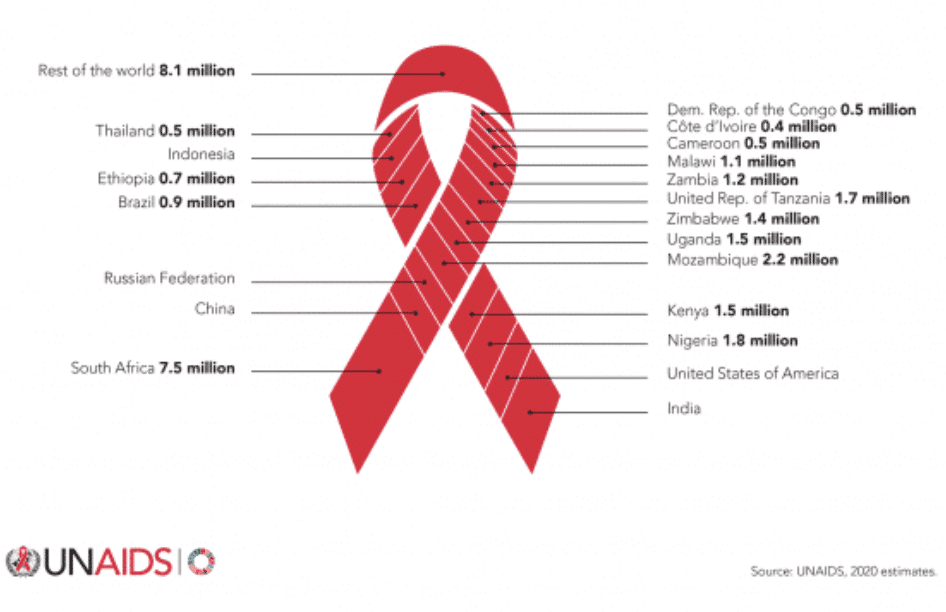
38 million people are living with HIV around the world
ART saves lives, but cannot cure HIV infection
Without medical intervention, HIV infection is inevitably lethal. ARTs have slowed the rate of new infections and reduced the number of deaths since the 2004 peak. However, these medications significantly impact quality of life, and the stigma of infection persists. Globally, there are approximately 38 million people living with HIV who would benefit from a cure, so why isn’t there a cure yet? In short, curing HIV is extremely difficult. To explain why, we’ll list the top five challenges in HIV cure research, then we’ll talk about how new gene therapy techniques may finally push HIV cure research over the finish line.
1. HIV is a retrovirus with a high mutation potential
Retroviruses, class VI in the picture below, are unique because of their ability to exist in RNA form, then transition to a DNA form to become a permanent part of the cell they infect. The cell can then read the DNA “master copy” of HIV repeatedly and make new RNA versions of HIV to export to other cells. During the transition from RNA to DNA and DNA to RNA, errors can occur, giving retroviruses like HIV the high mutation rate of an RNA virus with the permanence of a DNA virus.
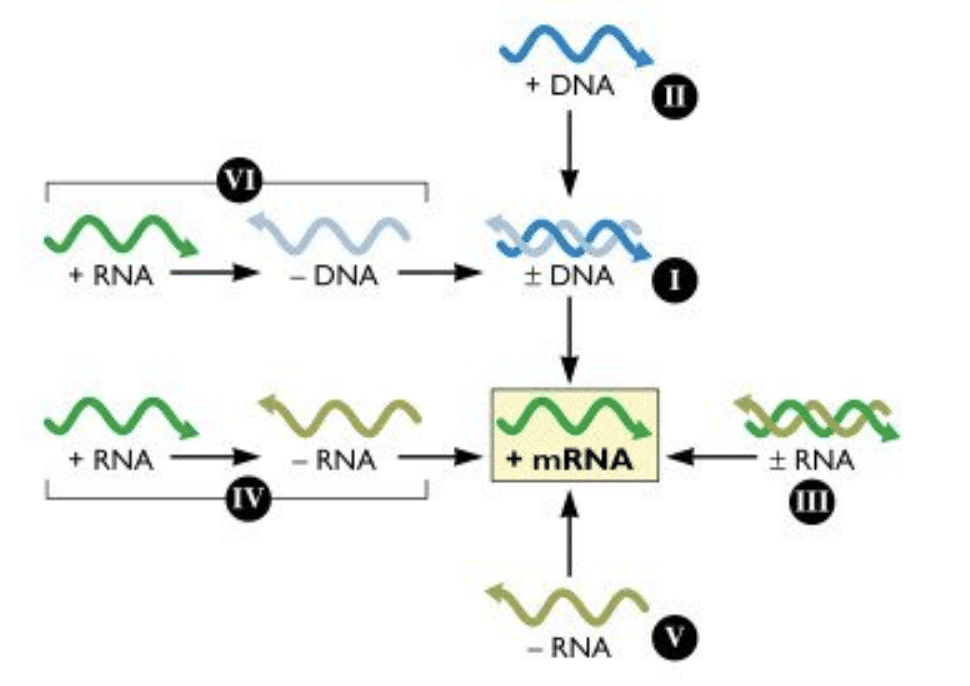
Figure 1: The Baltimore System, as illustrated by Dr. Racaniello, host of This Week in Virology, a staff favorite at Addimmune
In the 2017 paper, Recent Advances in Understanding HIV Evolution, Andrews and Rowland-Jones comment on the mutation potential of HIV: “HIV evolves extremely rapidly, exhibiting the highest recorded biological mutation rate currently known to science.” The mutation rate allows for the rapid generation of a wide diversity of HIV variants, which the authors identify as “a major contributing factor in the failure of the immune system to eradicate the virus.”
2. HIV infects immune cells
Another major hurdle to curing HIV is that the virus infects and adversely affects immune cells, the very cells that are required to fight an infection. HIV mainly infects the subset of immune cells called CD4+ “helper” T cells, which play a central role in the immune system. So, when HIV kills helper T cells, it causes immunodeficiency. T cells are mobile, heterogeneous, and capable of rapid cell division, making them ideal hiding places for HIV. Additionally, since HIV can hide in the DNA of a helper T cell, when the cell divides, its daughter cells carry the HIV genome, creating new HIV-infected cells without the need for cell-to-cell spread of HIV.
The T cells of the immune system divide in response to pathogens, so ironically, T cells that are meant to fight HIV manufacture more HIV-infected cells and become a major source of the virus in the body. Once HIV destroys the T cells which are responsible for the anti-HIV response, it can replicate unchecked and deplete the rest of the helper T cells, causing AIDS and opening the body to opportunistic infections and certain forms of cancer.
3. HIV establishes latent reservoirs
Viral latency is another major obstacle to an HIV cure. In a nutshell, latency is when a virus infects a cell but does not immediately begin creating new viral copies. Latent, resting HIV-infected cells can remain in “reservoirs'' in the body for months, or even years and become active at any time. Since current antiretroviral treatments (ARTs) target HIV itself, these medications are unable to eliminate latently infected cells because they are not actively producing viral particles. For the same reason, latently infected cells cannot be identified and eliminated by the immune system. Thus, eliminating the reservoir is the biggest challenge for the scientific community.
In a recent ScienceDaily article, the latent reservoirs were deemed “the main obstacle to curing HIV/AIDS.” The article details work done by a team of Gladstone visiting scientists, led by Nadia Roan, in which a set of cells were identified that “preferentially support latent infection by HIV.” The cells have a surface protein, CD127, and are “found in tissues such as lymph nodes…” Roan concluded, “our findings suggest that CD127 cells from tissues may be an important population to target for an HIV cure.” As further research is conducted to identify all of the sneaky places where HIV hides, one thing is certain, a full functional cure for HIV would need to address the infected cells of the viral reservoirs, whenever they show themselves.
4. Cure vs eradication
While ARTs are not a cure, this cocktail of drugs halts the progress of HIV to AIDS by targeting HIV at different stages of its replication cycle. Modern ARTs make it possible for those with HIV to live a nearly normal lifespan with the caveat that they must take medication on a regular basis while living with uncertainty over HIV’s reemergence – turning HIV from a death sentence to a life sentence. Since ARTs can be used to halt disease progression and minimize transmission, the continuous use of ARTs, in lieu of the search for a cure, forms the basis of most approaches to eradicating HIV.
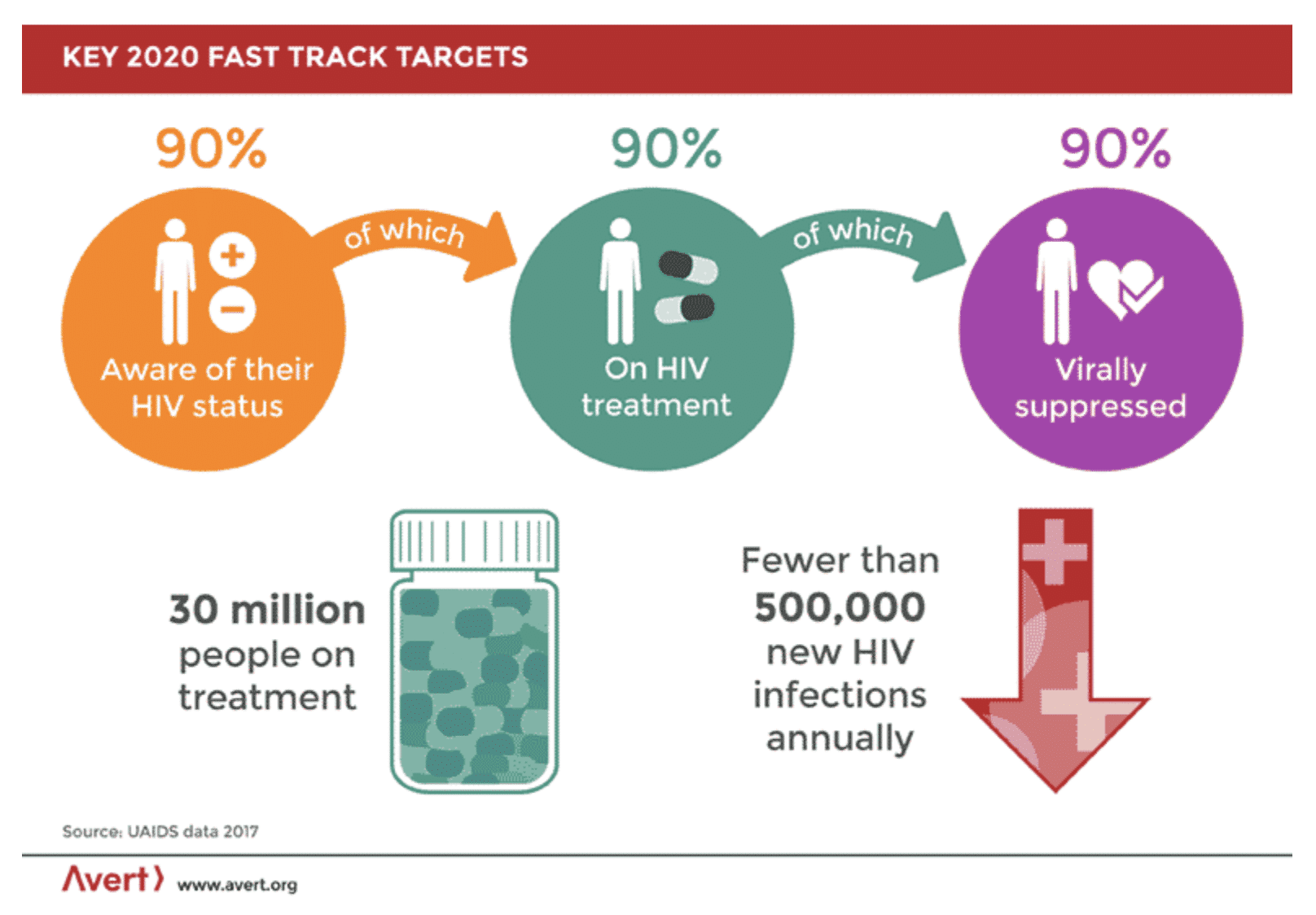
The UNAIDS 90-90-90 target for the “post 2015 era” approaches the HIV epidemic from a public health perspective and aims to eradicate HIV by 2030. By minimizing new infections, it is possible to eradicate a disease without the existence of a cure. In fact, that’s how we got rid of smallpox. UNAIDS sets forth a series of targets calling for people to first gain awareness of their HIV status, then to begin treatment, and then to suppress the virus through the use of ARTs and behaviors informed by their HIV status. While this approach does not provide aid to those already living with HIV, it is expected to control the spread of HIV, making it less and less likely that new infections will occur.
However, a shortcoming of the move to eradicate rather than cure is that in times of upheaval, such as that caused by COVID-19, efforts to work toward eradication are in danger of being sidelined. In May 2020, the UN issued a “wake-up call” to remind global leaders of the ongoing need for treatment in areas of the world where the largest loss of life is most likely to occur if the spread of the disease is not prevented. Eradication is a positive goal for preserving life for future generations; but again, it is not a cure for the 38 million people currently living with HIV.
5. The word “cure” has two definitions in HIV science
It seems simple enough to agree on what an HIV cure is, yet there are two different types of cures envisioned. Theoretically, if it were possible to eliminate all traces of HIV from the body, such an approach would be called a sterilizing cure. The other type of cure is a functional cure, in which the levels of HIV in the body would be kept below the level of detection without the use of antiretroviral therapy (ART). In the case of a functional cure, the infected person would not need to be on antiretroviral medication, would not experience the effects of HIV, and would not transmit the virus to anyone else. This is a cure because there would be no need for ART – ever – as opposed to a remission, in which there might be a recurrence of the disease.
Researchers have been searching for both types of cures for decades, and Addimmune’s ongoing human trials for a functional cure showcase the progress that has been made through the years. Our approach builds on the lessons learned from case studies like that of the Berlin patient and the London patient, who were declared cured of HIV, as well as previous genetic approaches to HIV such as Sangamo’s SB-728-T.
Conclusion - Why is it so hard to cure HIV?
A cure for HIV/AIDS has eluded researchers for decades. The virus’ interactions with the immune system make it difficult to cure since HIV can commandeer the T cells which are responsible for defeating it. This reduces the number of T cells directing an effective anti-HIV response and turns them into HIV sources. HIV also mutates at one of the fastest rates known to science, so far making it impossible to treat with a single drug. The virus can also hide, latent, in infected cells for long periods of time to escape detection.
The lack of agreement on how to approach the HIV epidemic splits resources between cure research and public health approaches. The potential diversion of funds to eradication over a cure is likely to leave the lifelong use of ARTs as the only recourse for people living with HIV. While reducing the number of HIV infections has a positive impact on public health, for those living with HIV/AIDS a cure would be life-changing. Further disagreement between what counts as a cure, and what language should be used to describe curative therapeutics adds additional complexity to creating solutions for the HIV epidemic.
For Addimmune, the goal is clear: prove that HIV can be functionally cured in a safe, scalable manner. HIV is a curable condition, as exemplified by cases like the Berlin patient and the London patient. These cases show us that under certain conditions, if the immune system has HIV resistance qualities, it can control HIV even if it reemerges from tricky hiding spots in the future. The next logical step is to use gene therapy to deliver HIV resistance genes to immune cells, which brings us to the ongoing clinical trials for AGT103-T. The fight against HIV has raged for over 4 decades, 32 million lives have been lost, and 38 million people are suffering in silence. We’re fighting for a cure, to liberate millions, and we invite you to fight with us. Use your voice to call for a cure.
Additional Questions
Thanks for reading to the end! Here are some common follow-up questions:
Question: Can HIV be cured?
Answer: Yes! HIV has been declared cured before, but only under special circumstances. The next step in HIV cure research is to develop a safe, scalable method.
Question: Why is it so hard to cure HIV?
Answer: HIV is a tricky virus that entangles itself with the immune system. Modern medication can effectively block HIV replication but cannot separate the viral DNA from the immune system.
Question: Why is HIV so hard to treat?
Answer: HIV infection is often asymptomatic, so it is difficult to identify before the virus does damage to the immune system. Additionally, HIV mutates very quickly, so doctors need to consider the possibility of antiviral resistance.