A Noble Pursuit: Gene Therapy for Rare Disease
Rare disease, as the name suggests, affects a small proportion of the population and appears with low prevalence. The limited number of patients impedes development of new therapies, reducing the pool of clinical trial candidates and the size of the end market. A surprising figure is that the average rare disease has a population below 100. According to the National Institutes for Health, there are ~7,000 identified rare diseases; however, most do not have any approved treatment. The agency further notes that over 80% of rare diseases have a monogenic cause.
While there are many drugs for rare disease, successful gene therapies provide a contrast to the chronic nature of conventional treatment. In some cases, one application of gene therapy may provide a cure to a disease that would otherwise require ongoing therapy. With favorable regulatory structures, advancements in gene sequencing and a number of precedent medicines in rare disease, gene therapy is a strong contender for providing solutions.
Is Gene Therapy Economically Feasible?
The process for developing and bringing medicines to the market is complex, costly, and requires the collaboration of researchers, industry, patients, medical professionals, investors, funding bodies and regulators. While it may appear that allocating resources to rare disease is an inefficient use of resources, this is not necessarily true. This prima facie economic argument fails to recognize the physical and mental toll of rare diseases, which are frequently more serious and lack the medical support of more common disorders. Furthermore, from a purely economic standpoint the systematic cost of care for rare disease patients is up to five times greater compared to others. Rare diseases also skew towards children, who can benefit over a longer potential lifespan.
Why Rare Diseases Are Overlooked
Rare diseases have several features that differentiate them from more common conditions, leading to a lack of attention. Due to limited frequency, there is often an extended period where there is either no or an incorrect diagnosis which can delay treatment and increase the risk of complications.
Orphan diseases receive a lower allocation of research efforts and resources, making them inconspicuous for both the layman and medical community. Additionally, it’s difficult to populate clinical studies to further investigate the rare disease as there are fewer patients available.
These factors lead to a scarcity of approved treatments. If medicines do exist, they are expensive and frequently only address the symptoms of the disease. This can leave patients with few options for managing their condition.
Rare Diseases and the Orphan Drug Act
In the early 1980s, many stakeholders recognized that the lack of treatments for rare disease was a pressing need and, in response, the Orphan Drug Act was passed in 1983. This legislation provided a broad array of incentives for investment in rare disease development. According to the National Institutes of Health, in the 36 years since it was enacted, 600 orphan drug indications have been granted approval from 450 different drug products, an average of almost 17 per year. This compares to only 10 approvals in total for rare disease drugs in the decade prior to the passage of the legislation, or an average of one per year.
Cumulative FDA Approved Orphan Indications and Drugs
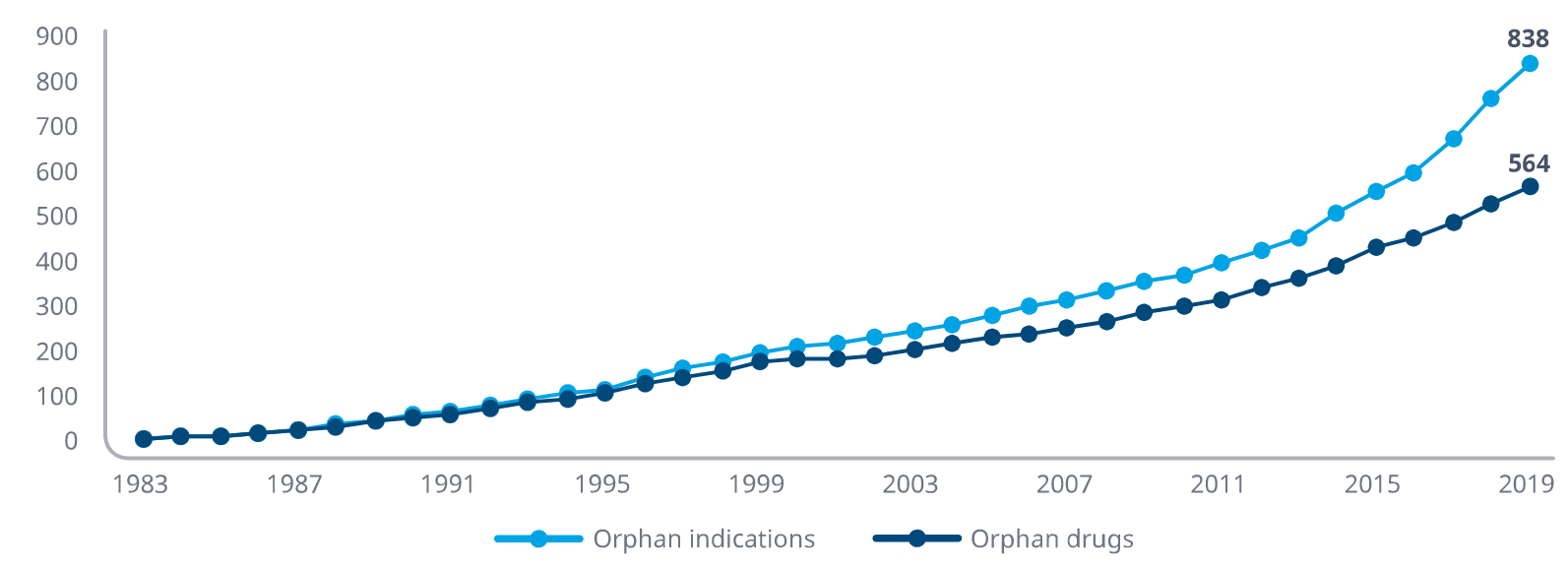
Source: IQVIA Institute for Human Data Science
Incentives to Offset High Costs
The cost of rare disease therapies is high. Several factors are behind the premium, primarily arising from the need to spread development expenses over a smaller population. Key drivers include high per-patient clinical trial costs given the small population that must travel to distant trial site locations and few physicians able to diagnose and manage the process. The high cost of manufacturing specialized drugs that lack economies of scale is another consideration.
To offset the steep costs, many incentives are available which offer modified regulatory pathways and economic inducements to life sciences companies to help increase the number of treatments available. The benefits vary by country but generally offer product exclusivity, tax credits and grants. We list several of the incentives, by country, below.
Summary of Rare Disease Development Incentives, by Country
| Benefits | US | EU | Australia | Japan | China |
|---|---|---|---|---|---|
| Criteria | Cost not reasonably recoverable | Life threatening & chronically | Serious condition, financially unviable | No alternative, high efficacy | Significant impact, diagnosable |
| Definition | <200,000 | <5/10,000 | <1/2,000 | <50,000 | <1/10,000 |
| Approval | Accelerated | Expected review | Priority review, provisional approval | Clinical trial waivers, priority review | Clinical trial waivers |
| Exclusivity (years) | 7 | 10 | 10 | 10 | 6 + possible extension |
| Tax Incentives | Tax Credits | Tax Credits | R&D incentive | 12% tax credit | 50% R&D tax credit |
| Research Subsidies | NIH Grants | Numerous | Grants, funding programs | Yes | Yes |
| Other Incentive | Priority review voucher, fee waivers | Fee reductions, protocol assistance, guidance | Fee waivers | Fee reduction, regulatory guidance | Reduced VAT |
Source: Author compilation of details from various government and private sources
Why Gene Therapies are Better Suited for Treating Rare Disease
Gene therapy has several characteristics which make it a smart choice for treating rare disease. Repairing or replacing defective genes is a highly repeatable approach which, once mastered, can be applied to a wide variety of genetic diseases. Gene therapy can frequently provide a cure, repairing the genetic defect and freeing patients from lifelong disease and the need for symptomatic or disease modifying treatment.
Gene therapy introduces genetic material into a patient’s cells to correct or compensate for a defective or missing gene. This is achieved through the delivery of a functional copy of the gene sequence in place of the defective component. There are several methods for delivering therapeutic genes to cells, which include viral vectors, non-viral vectors and electroporation which depend on the type of disease being targeted. The complexity of the approach arises more from the delivery of the desired gene sequence rather than finding the right gene sequence.
In the context of rare diseases, gene therapy can be particularly promising because many rare diseases are caused by a single genetic mutation. By correcting or compensating for this mutation, gene therapy has the potential to provide a long-term, potentially curative treatment.
Gene Sequencing
Gene sequencing was first successfully completed on a human in 2003. It took thirteen years as part of the Human Genome Project and cost as much as $1 billion. Based on the latest technology offered by Illumina and Ultima Genomics, a human genome can now be decoded in a few hours at the cost of a few hundred dollars.
Genome sequencing has simplified the diagnosis and identification of rare diseases. Genetic testing allows scientists to find genetic mutations that cause disease. Genome sequencing has also enabled the medical community to identify thousands of disease-causing genes, thereby improving our understanding of underlying disease mechanisms. It can also help identify individuals before the rare disease manifests itself, allowing treatment to begin early and potentially sidestepping the effects of the disease altogether.
The ease of obtaining an individual’s genetic makeup through whole genome sequencing (WGS) allows for rapid diagnosis of many rare diseases that otherwise might not be identified. WGS can save years of doctors’ visits and confusion over undiagnosed symptoms. In a recent study of rare disease, 40% of cases were able to be molecularly diagnosed.
Rare diseases have traditionally been diagnosed using clinical experience gained from prior exposure and reliance on medical literature. With symptoms that a physician may only see once or twice over a career, many patients remain undiagnosed and may even die without a diagnosis. As genetic and exome sequencing has become more accessible and affordable, it provides an efficient tool to establish the genetic cause and identify a gene therapy solution.
Gene Therapies for Rare Disease
There are many examples of what appear to be initially expensive gene therapies reducing the overall cost of rare disease. We share three recent examples where the upfront cost of gene therapy is in the millions; however, it is less than the lifetime expense of ongoing care, because the gene therapy is a curative one-time treatment. When the non-economic benefits are added from alleviating the burden and suffering of the patient who otherwise requires constant infusions and experiences only temporary relief, the argument is even stronger.
Zolgensma
Approved in 2019, Zolgensma is a gene therapy that commands a price of $2.1 million to cure spinal muscular atrophy (SMA). It is a one-time treatment that can allow patients to sidestep ongoing treatments such as risdiplam that would cost $3.4 million for ten years of treatment or nusinersen which costs over $4.1 million for 10 years of therapy, in addition to the cost of spinal injections. Despite Zolgensma’s shockingly expensive price tag, it can save the system money overall and allows for better patient health.
Hemgenix
CSL Behring received FDA approval for its hemophilia B gene therapy Hemgenix in November 2022 and subsequently announced a price of $3.5 million. It was the first gene therapy treatment for hemophilia, which is a severe disease where patients can suffer from prolonged or heavy bleeding after injury, surgery or for no apparent reason due to the lack of a clotting factor. According to an article in Managed Healthcare, annual cost of symptomatic treatment of hemophilia B is from $300,000 to over $700,000 per year requiring multiple weekly infusions. With Hemgenix, the one time treatment can replace the missing gene for clotting Factor IX, providing a long term cost reduction to the health care system and a substantial quality of life improvement to patients.
Zynteglo
Another headline grabbing price tag made the rounds in fall of 2022 with Zynteglo asking $2.8 million per treatment. The drug is bluebird bio’s cell-based gene therapy for patients with beta-thalassemia. This condition is a type of inherited blood disorder that causes a reduction of normal hemoglobin and red blood cells in the blood, leading to insufficient delivery of oxygen in the body. Similar to the other gene therapies mentioned here, Zynteglo is a one-time gene therapy product administered as a single dose which adds functional copies of a modified form of the beta-globin gene to a patients hematopoietic stem cells allowing them to make normal hemoglobin. Prior to the availability of Zynteglo, patients would receive a regular blood transfusion every two to five weeks at an average annual cost of almost $130,000 in 2018.
Challenges
Viral vectors
The viral vectors commonly used in gene therapy to deliver therapeutic genes to target cells in the body may only reach the desired cells and tissues with difficulty. Some viral vectors may not penetrate certain tissues or can activate an immune response, thereby limiting effectiveness.
Additionally, the delivery method for viral vectors can vary depending on the disease being treated and the target tissue. For example, using a viral vector to deliver a gene to the brain to treat a neurological disorder may require invasive surgery, while delivering to the lungs to treat a respiratory disease may require inhalation therapy. The difficulty arises from the administration method rather than the gene sequence.
Immune system responses
New gene sequences may produce proteins that the immune system does not recognize, and these may be attacked and removed by the immune system, eliminating the gene therapy benefit and causing a severe reaction. For a durable treatment, gene therapy should be integrated into the cells that are responsible for the targeted protein. If it is not integrated and consists of plasmids, for example, divided cells will not pass on the modification to daughter cells and additional doses will be required.
Other challenges
There are additional concerns related to understanding the disease mechanism and unintended consequences of the changes. Other considerations include manufacturing and quality control as well as regulatory and ethical considerations. Despite these challenges, numerous gene therapies for rare disease have been approved.
Final Diagnosis
Gene therapy is particularly relevant to rare disease, as an estimated 80% of rare diseases are monogenic. Traditional drugs frequently work by treating the symptoms rather than the underlying cause. When there is a monogenic source, it is feasible for gene therapy to repair the underlying damage. Another benefit of gene therapy is that it can be a “one and done” treatment, in contrast to ongoing chronic therapy.
The value of the technology is not in the gene sequence that needs to be replaced, but rather in the vector that is used to transport it. If a gene sequence can be successfully delivered to a type of tissue, many diseases that arise from a genetic source can be addressed. The gene sequence can be framed as a commodity that can be inserted to address a wide variety of diseases and the delivery vector becomes the technology that gives it value.





